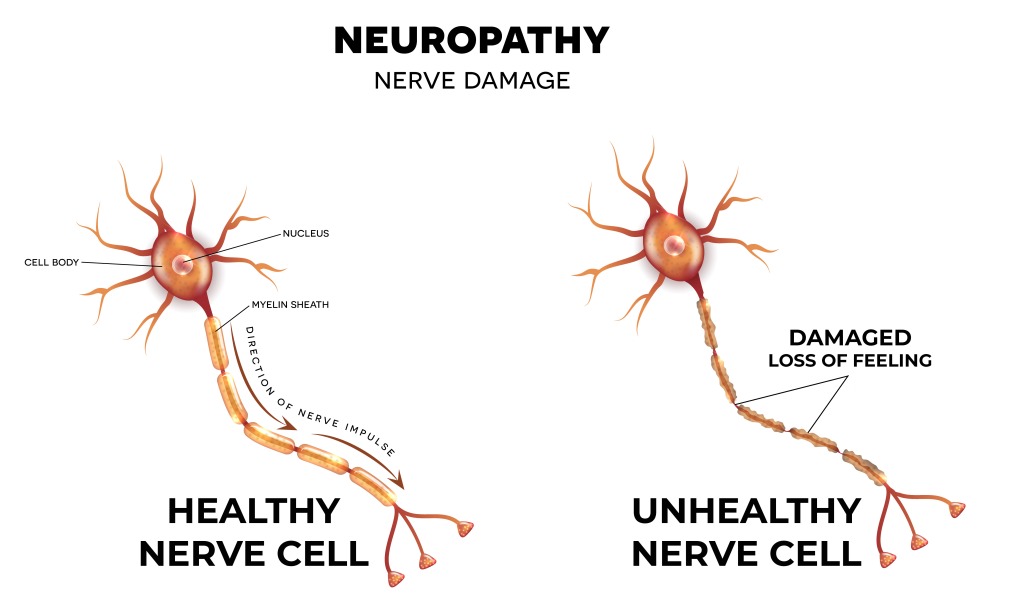
Approximately 350 million people worldwide have arthritis. Arthritis is a condition defined by painful inflammation and stiffness of the joints. Exercise may be the last thing on a person’s mind when suffering from arthritis. But exercise is absolutely crucial. A person may think exercise will aggravate their joint pain and stiffness, but that’s not the case. Lack of exercise can actually make your joints even more painful and stiff.
EXERCISE CAN…
-
- Strengthen Muscles Around Joints
- Help Maintain Bone Strength
- Give You More Energy
- Help Control Your Weight
- Enhance Your Quality of Life
- Improve Your Balance
Keeping muscles and surrounding tissue strong is crucial to maintaining support for your bones. Not exercising weakens those supporting muscles, creating more stress on your joints. Exercise is considered the most effective non-drug treatment for reducing pain and improving movement in patients.
How Therapy Can Help You!
Exercise is extremely important in managing arthritis symptoms, but it may be hard to get started and maintain an exercise program. Overcoming the hurdles of pain, exhaustion, or boredom can be difficult, especially on your own. A physical or occupational therapist can help you to overcome these hurdles and gain success in maintaining your exercise routine. Physical therapists evaluate your needs and teach you how to exercise appropriately for joint mobility, muscle strength, and fitness. Physical therapists can also recommend exercises for you to do on your own. These exercises might include; range-of-motion exercises, aerobic exercises, and strength training. Occupational therapists help by teaching you how to protect and reduce stress on your joints while exercising and performing daily tasks. Talk with your doctor about the benefits of both physical and occupational therapy for your arthritis needs!