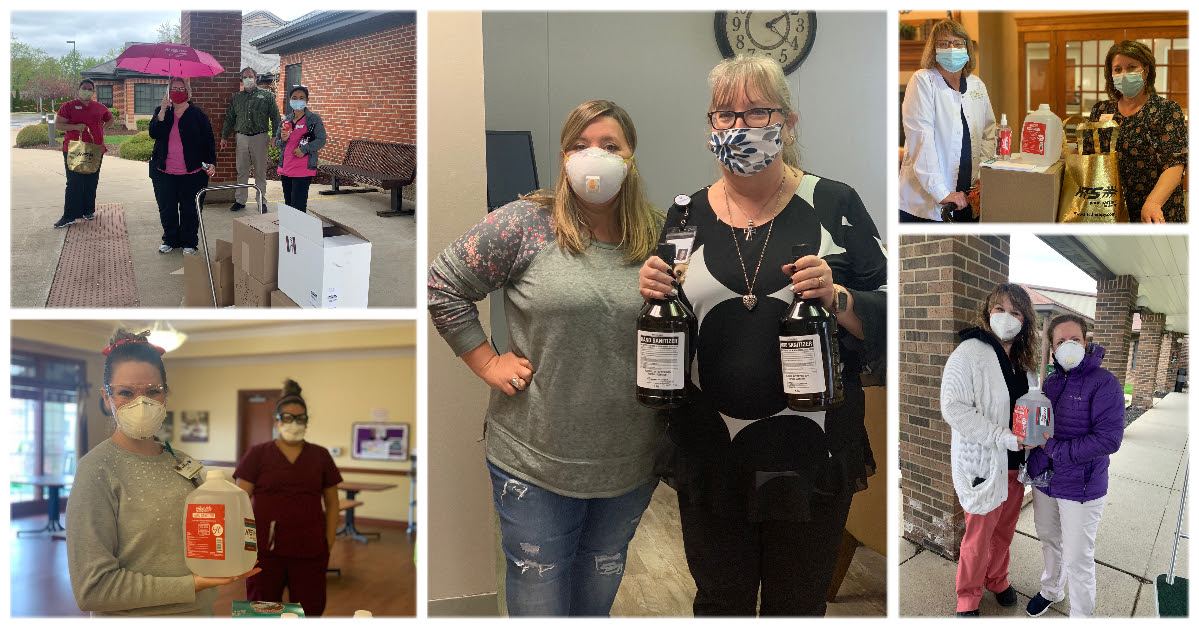
Last week, HTS held a Nurse Appreciation contest to celebrate National Nurse’s Week! Thank you to everyone for sending in nominations. We are honored to work alongside so many wonderful nurses in our communities. Thank you for your sharing your incredible hearts and devoting tireless service to our industry.
Our Nurse’s Week Winners Are…
Each winner will receive a $50 gift card and swag bag from your friends at HTS.
Ashley Plue, LPN at Milner Community Health Care
Alison Snow, Director of Nursing at Nazareth Home Clifton
Cassandra Brown, RN BSN Director of Nursing at Metcalfe Health Care Center
Barb Sword, RN, HFA, CDP Director of Clinical Services at Hickory Creek
Christy Canter, RN at Hickory Creek at New Castle
Laurie Briggs, LPN at Grayson Manor
Katrina Wilson, Director of Nursing at Guerin Woods
Kelly McDougal, Health Services Director at Crestwood Village South
Michelle “Missy” Ryan LPN, MDS Coordinator at Northview Health & Living
A Special Shout Out to All the Amazing Nurses Nominated!
As a special thank you to all the nurses nominated, HTS will be sending each nurse a small gift from us to express our sincere appreciation and gratitude.
Alicia Tankersley at Swiss Village
Alma Ahmetovic at Swiss Village
Barb Simpson at Good Samaritan Home
Cynthia Palm at Maple Manor
Dana Roach at LLV Pine Valley
Debbie Rohrig at Ripley Crossing
Delisa McCloud at Glenburn Home
Heath Haver at Golden Years
Jaymee Brockhaus at LLV Pine Valley
Jayne Melton at Ketcham Memorial
Jessuca Willis at Hickory Creek at Hicksville
Kate Molin at Golden Years
Kelly Badjek at Hamilton Grove
Kim Davis at Heritage Pointe of Huntington
Kim Ray at Spring Creek
Kim Smith at Golden Years
Kristy Uhrick at Swiss Village
Mandy Bonbrake at Heritage Pointe of Huntington
Megan Rittenhouse at Heritage Pointe of Huntington
Monica Broady at Maple Manor
Nada Wireman at Parkview Haven
Natalie Bergman at Compass Park
Nicole Kubley at Grace Village
Pam Grabbe at Golden Years
Patty Engle at Ripley Crossing
Rona Westrich at Hamilton Grove
Sandy Stearns at Metcalfe Health Care Center
Sharon Smitty at Guerin Woods
Shona Kirkpatrick at Golden Years
Steve Brian at Guerin Woods
Teresa Headington at Guerin Woods
Teresa Medler at Good Samaritan Home
Theresa Wright at Golden Years
Tressa McNeely at HIckory Creek at Scottsburg
Viola Sheckles at Hickory Creek at Franklin