On April 12. 2021, the Indiana Department of Health, Division of LTC will resume federal and state health surveys for both nursing homes an residential care facilities. All surveyors have been updated with the Long-term Care Survey Process (LTCSP) Procedure Guide that was effective February 6, 2021. Surveyors will review facility information 12 months prior to the survey entrance date, unless there is a need related to complaint or other concerns that would require information past the 12-month time frame.
On April 9, 2021, CMS issued a new Memo to State Survey Agencies (QSO-21-17-NH) resulting in an end to a few waivers which were granted under the PHE.
The below flexibilities will end effective 5/10/2021:
- The emergency blanket waivers related to notification of resident room or roommate changes, and transfer and discharge notification requirements
- The emergency blanket waiver for certain care planning requirements for residents transferred or discharged for cohorting purpose
- The emergency blanket waiver of the timeframe requirements for completing and transmitting resident assessment information Minimum Data Set (MDS)
Changes in QSO-21-17-NH were updated on April 8, 2021 and made available to providers via this link: COVID-19 Emergency Declaration Blanket Waivers for Health care Providers. Please note, waivers that will end effective 5/10/2021 are found on pages 18-19 of the linked document are in red, strikethrough font
On April 8, 2021, CMS released the new Skilled Nursing Facility (SNF) Prospective Payment System (PPS) Proposed Rule which, once finalized, is effective October 1, 2021. This proposed rule updates Medicare payment policies for facilities under SNF PPS for fiscal year 2022. The proposed rule also includes information for the SNF Quality Reporting Program (QRP) and SNF Value-Based Program (VBP) for FY 2022.
See below for the most significant areas of updates:
- FY 2022 updates to the SNF payment rates
- Methodology for recalibrating the PDPM parity adjustment
- Rebase and revision of the SNF market basket to improve payment accuracy under the SNF PPS
- New Blood Clotting Factor Exclusion from SNF Consolidating Billing
- Changes in PDPM ICD-10 Code Mappings – The ICD-10 code mappings and lists used under PDPM are available on the PDPM Website at: https://www.cms.gov/Medicare/MedicareFee-for-Service-Payment/SNFPPS/PDPM
- SNF QRP update – modification to the public reporting SNF quality measures
- SNF VBP Program proposal to suppress the SNF readmission measure
For more information on this proposed rule, please visit the Federal Register’s Public Inspection Desk under “Special Filings,” at http://www.federalregister.gov/inspection.aspx.
Do you often wake up feeling stiff and sore in the morning? Do you have trouble getting out of bed or walking into the kitchen to get your breakfast? This is commonly known as morning stiffness that is caused by worn joints, muscle tightness, or arthritis. We feel this tightness in our bodies more frequently in the morning due to the hours of inactivity while sleeping. The area of stiffness varies by person, but most say in the morning is when it feels the worst. Research shows pain will subside about an hour after waking or soon after moving.
To help ease morning stiffness, keep these tips in mind…
- Medication: Keep pain-relieving or anti-inflammatory medications by your bedside and take them 30 minutes prior to getting up.
- Arm & Leg Circles: Moving arms and legs gently in a circular motion while lying in bed can help relax muscles and get the blood circulating.
- Stretching: While still lying in bed, incorporate stretches that target the stiffest areas of your body including the back, hips, knees, and shoulders.
- Heat: Before or after stretching apply a heating pad or take a hot bath to help loosen tight muscles and make it easier to get moving.
- Joint Cream: Putting joint cream on specific areas of tightness can provide short-term relief and make it easier to move and stretch.
- Herbs and Supplements: Herbal treatments like fish oil, evening primrose, borage, or black currant oils may ease joint stiffness and inflammation from arthritis.
If morning stiffness affects your ability to safely get out of bed or is keeping you from enjoying activities, talk with your doctor about the benefits of physical and occupational therapy.
How Can Physical & Occupational Therapy Help?
After a thorough evaluation, therapy may recommend different sleep positions and exercises to improve flexibility, strength, and range of motion. Additional specialized treatments may include hot and cold therapy, therapeutic massage, and the use of pain-reducing technology such as electrical stimulation and ultrasound therapy.
HTS has identified the top 5 therapy clinical outcome focus areas for 2021 based on our experiences from 2020 which makes us better equipped to overcome COVID-19 related obstacles. Furthermore, after attending a 15-hour training and certification process, HTS management staff have all become “PDPM Masters.”
These additional “feathers in our cap” allow us to uniquely champion process improvement initiatives alongside your interdisciplinary team. As HTS continues to identify opportunities for clinical growth, we look forward to discussing these key process improvement areas in the coming months.
Top 5 Therapy Clinical Outcome Focus Areas:
- Working Smarter with Workflow Processes
- PDPM Case Mix
- Medicaid CMI
- Section GG Outcomes
- Part B Programming
*In February, we announced all HTS Regional Directors and Assistant Regional Directors earned their PDPM Master Class Certification. This 12-month course for skilled nursing facilities was offered through Leading Age Indiana in 2020. The certification process included 15 hours of training and competency assessment provided by nursing and MDS experts at Proactive Medical Review.
HTS supports our valued partners with access to high demand IDT toolkits, trainings, and many other process improvement resources conveniently available on HTS PartnerHQ web portal. Not a partner? Contact us to discuss how your community can be part of these focus outcome discussions.
Blog by: Jessica Duffy, OTR, Regional Director, Healthcare Therapy Services, Inc.
The word relationship is defined as: “The way in which two or more concepts, objects, or people are connected, or the state of being connected.” I think it is fair to say that COVID has completely changed how many of our interpersonal and working relationships operate now. As we look at this from a higher perspective, however, what has that really changed for us?
When I think of the relationships that are very important in our life, I am acutely aware of the importance of being present. For example, as a mother, it is not an option for me to miss any of my children’s events. I would not be happy with just getting the “rundown” after the big game; I would want to experience it with them first hand! Who wants to hear the exciting tale of making the game point–an hour after it occurred?! Not me. I want to see it and experience it. There is power in being present. This power and concept of being present applies in our professional lives as well. Let’s discuss how we can be present at our workplace.
With all of the new regulatory changes, quarantining, the elimination of group gatherings, etc., it has become all too easy to lose track of some of the systems we have in place to continue relationships in our buildings. We have at times, just given a document or report, in lieu of having our normal meeting because it more readily meets the demands of COVID-19 restrictions. Perhaps in a larger site, we stayed only in the healthcare area to prevent cross-contamination. I’m sure as you read this, ten more scenarios have popped in your mind of how we have changed our operations, but is what we are doing right or even optimal? Is it truly meeting that need of “staying connected”?
As in my parenting example, would you be ok with just getting the report of your child’s big event, or would you somehow finesse the opportunity to be more personally present? If entry is not permitted, is it live-streamed? Can you Zoom, Facetime, etc.? I have done it all, by the way, this past year. As a proud sports mama, I have watched live-streamed sporting events through the school and Zoomed my children’s teammates or coaches who could be at the event so that I can experience it firsthand while working in the red zone.
When it comes to our clients and our daily operations, HTS Therapy chooses to be PRESENT. Instead of assuming it is ok to substitute a connection, such as the morning meeting, a clinical or Medicare meeting by simply passing out forms, we want to finesse that personal interaction. If an in-person meeting is not an option, then we will leverage a virtual meeting or conference call. Our team believes best practices happen through an interdisciplinary team collaboration.
HTS Therapy chooses to be present.
Need a Powerful Therapy Partner? Contact Amanda Green, Executive Director of Strategic Development amanda@htstherapy.com for information about our contract therapy partnerships.

Jessica Duffy, OTR
Regional Director | Healthcare Therapy Services, Inc.
Post COVID-19 Rehabilitation Program
The HTS Post COVID-19 Rehabilitation Program was created by HTS clinical staff to improve strength, endurance, balance, activity tolerance, functional mobility, swallowing, and cognitive-communication… all of which can be adversely affected during the COVID-19 recovery process.
This program will help those individuals who are recovering from COVID-19 and are unable to return to the daily tasks they were able to complete at a prior level of function.
Achieving the highest possible quality of life and independence with the use of therapeutic exercises and training are used to facilitate successful COVID-19 recovery.
Who Can Benefit From This Program?
The Post COVID-19 Rehabilitation Program can benefit those who have recovered from COVID-19 and are experiencing lingering health issues, such as:
- Poor Endurance
- Decreased Activity Tolerance
- Muscle Weakness and Decreased Strength
- Inability to Complete Daily Tasks when Compared to Prior Level of Function (walking or moving from bed to chair)
- Difficulty Swallowing (coughing, choking, excessive throat clearing, swallowing pain)
- Memory Problems or Difficulty Focusing
- Soft Voice Difficult for Others to Hear
- Difficulty Finding Words During Conversation
HTS Therapists are equipped with the knowledge and training to provide this critical treatment intervention to help patients achieve a successful COVID-19 recovery. For more information about the HTS Post Covid-19 Rehabilitation Program, please contact your HTS Regional Director.
Need a Powerful Therapy Partner? Contact Amanda Green, Executive Director of Strategic Development amanda@htstherapy.com for information about our contract therapy partnerships.
Why is hand and grip strength so important? Having a strong grip makes it easier to perform normal daily tasks like holding a coffee cup, carrying grocery bags, or brushing your teeth. Research has shown that a person’s grip strength can be an indicator for overall muscle strength, upper limb function, bone mineral density, increased fractures and falls, and overall quality of life.
It’s common as we age to see a decrease in grip strength due to natural age-related loss of strength and muscle mass. Additionally, other causes may include scar tissue, carpal tunnel, arthritis, and nerve or tendon damage. As a result, a person may experience trouble holding and opening items and other activities they enjoy.
Now that we recognize why grip strength is so important, below are exercises that can help to improve your overall hand and grip strength.
- Improve Crush Grip (ability to squeeze something between your fingers and palms) with hand strengthening equipment like stress balls, therapy putty, and hand exercisers.
- Improve Finger Strength & Dexterity with a finger-walking exercise. Put your hand on a table, palm facing down. Slowly lift each finger moving toward the thumb.
- Improve Support Grip (ability to hold on to an object) with farmer carries. Hold a weight or bag and walk with it across the length of the room, then turn around and walk back.
- Improve Pinch Grip (the grip strength between the tips of your four fingers and thumb) by pinching clothespins or using tweezers to manipulate small objects.
- Improve Hand Range of Motion with finger stretches. Put your palm down on the table, straighten your fingers, hold the stretch for 30-60 seconds, and release.
Physical & Occupational Therapy Can Help! If you are having difficulty with hand strength or pain due to weakness, injury, or illness, you may find that performing a simple task is troublesome. Physical therapists recommend exercises to improve range of motion, build strength, and regain function. Occupational therapists offer strategies to overcome challenges so you can fully participate in daily and leisurely activities.
Talk with your doctor about a prescription for outpatient therapy.
The COVID-19 virus has impacted the health of millions of people. Research studies have shown that COVID-19 affects your body in several different capacities. As pulmonary issues are the most widely known complication from COVID-19, the virus can also affect your heart muscles, brain function, muscle strength, activity tolerance, and overall functional mobility. If you had COVID-19, you may need therapy to get you back to good health.

Our Post COVID-19 Recovery Program helps individuals who continue to have lingering effects from a battle with COVID-19. Our program utilizes physical, occupational, and speech therapists to provide strength training that aims to restore lost muscle and exercises focused on improving lung function and activities of daily living. Our goal is to ensure you get back to an independent and active lifestyle.
Treatment can help improve:
- Strength
- Endurance
- Balance
- Mobility
- Swallowing
- Communication
- Memory
- Daily Living Skills (bathing, dressing, cooking, and cleaning)
In order to participate in this program, you must have a doctor’s order for therapy. For more information about this program, please contact your on-site Therapy Department to discuss your concerns and treatment options.
On December 2nd, the release of the CY 2021 Medicare Physician Fee Schedule Final Rule confirmed that we would face a huge overall 9% cut in our Med B Therapy CPT code reimbursement beginning January 1, 2021. I talked to many of you as we shook our heads and shared our mutual concern about such a large cut. The impact on our senior care providers and specifically, our rural locations would be devastating. It was clear that the outpouring of advocacy efforts in response to the fee schedule proposed rule were being ignored. During a pandemic, that has overwhelmingly impacted our geriatric population, our critical rehabilitation services were gravely at risk of not being accessible due to such significant reimbursement cuts.
Thankfully, our industry has once again proved to be irrepressible! Our associations, industry leaders, and stakeholders nationwide persevered by rallying together to fight for our rehab services to be regarded as essential and to reduce the financial impact that was imminent in the final rule. We at HTS, as an active member of NASL (National Association for Support of Long-Term Care), urged all of our therapy team members to fervently become part of the advocacy for our patients and our profession. Proudly, countless HTS employees reached out to our federal legislators to provide the necessary details of how this cut in reimbursement would affect our most vulnerable population during the PHE.
The outcry from stakeholders commanding legislative action to protect rehabilitative services paid off. In late December, Congress passed the Consolidated Appropriations Act of 2021 (H.R. 133). This provided a partial fix for the looming therapy cuts.
The overall impact to the Medicare B Therapy CPT codes was significantly diminished as a result of the provisions of this Act. Now, instead of an estimated overall 9% cut, therapy codes’ reimbursement will be reduced by approximately 3.5% (depending on the code). While this is still a financial hit in the midst of a pandemic, the ability for operators to compensate and adapt to lower reimbursement is more fathomable than the original 9% reduction. This partial fix is made possible by the following measures:
- The bill delays the implementation of the new add-on fee schedule complexity code (G2211) for three years.
- The bill infuses $3 billion into the 2021 fee schedule for one year only which adds 3.75% of payment for all codes.
- The bill delays the 2% Medicare sequester cuts for three months.
- The bill continues the current Alternative Payment Model thresholds for two additional years
- The bill extends the work 1.0 geographic index floor which increases payments for the work component of the physician fee schedule payments through December 31, 2023 for geographical areas that labor cost is lower than the national average.
Here is an example of commonly used therapy CPT codes illustrating the impact of the Consolidated Appropriations Act of 2021 (H.R. 133) for both the 9% and 3.5% reductions.
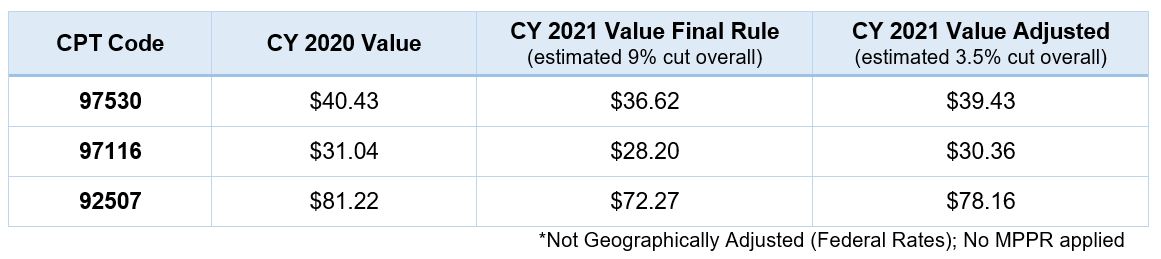
As shown in this example, providers and therapy companies alike will be challenged to offset the reduction in reimbursement. This offset may additionally be exaggerated by the overall increased costs associated with the pandemic. The need for PPE, COVID testing for employees, as well as reduced efficiencies due to isolation and other restrictions, will continue through the coming months as we continue to power through the most difficult challenge in our industry.
HTS will continue to stay steadfast during this time and true to our mission of providing “a hope and a future” (Jeremiah 29:11) to maintain the best quality of life for those we serve. Please contact me with questions, and we will continue to keep you updated on any changes on this topic and many others in the future.

Cassie Murray, OTR, MBA, QCP
Chief Operating & Clinical Officer
References:
https://rules.house.gov/sites/democrats.rules.house.gov/files/BILLS-116HR133SA-RCP-116-68.pdf
https://waysandmeans.house.gov/sites/democrats.waysandmeans.house.gov/files/documents/Overall%20Summary%20Joint%20Committees%20Final%2012.21.pdf
