Common Therapy & Billing Code Issues
Navigating UB04 coding can be tricky, especially with complexities like “Excludes 1” and “Excludes 2.” It’s up to billing departments and the triple check process to understand these nuances to avoid costly errors and ensure compliance with CMS and NCHS guidelines.
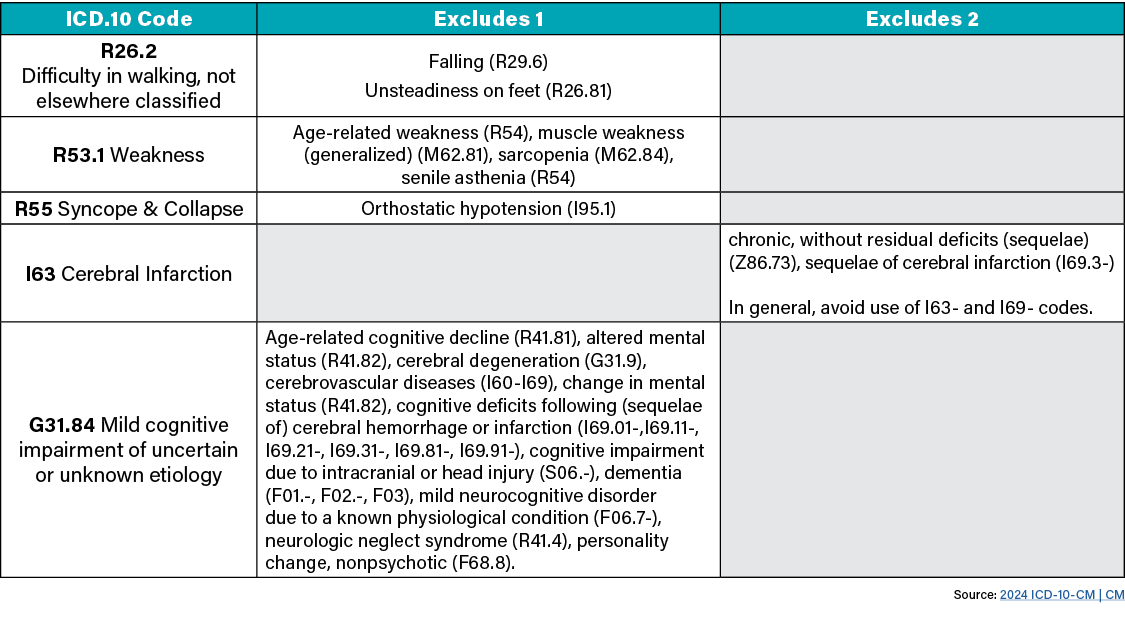
Excluded Notes
There are two types of excluded notes. Each type has a different definition, but they all indicate that codes excluded from each other are independent of each other.
Excludes 1: This means, “Not Coded Here!” The code excluded is to never be used at the same time as the code above the Exludes1 note. These types of codes are used when two conditions cannot occur together, such as a congenital form versus an acquired from of the same condition.
Excludes 2: This means, “Not included here.” The code excluded indicates that the condition excluded is not part of the condition represented by the code, but a patient may have both conditions at the same time. When an Excludes 2 note appears under a code, it is acceptable to use both the code and the excluded code together, when appropriate.
What Can We Do?
Per CMS, “The entire record should be reviewed to determine the specific reason for the encounter and the conditions treated.” Providers must ensure their triple-check process is as efficient and effective as possible to maintain clean and accurately coded claims with consistency across the record.
- Medical and Treatment Diagnosis Codes assure the UB-04 matches the MDS
- ICD.10 Codes assure the UB-04 matches the MDS
- Supportive Nursing Documentation
- UB-04 review sequencing of coding and that all date required is present
By adhering to these guidelines and diligently reviewing records, we can improve the accuracy of our coding, enhance compliance, and ensure optimal reimbursement for the care provided.



